OVERVIEW
Age related macular degeneration or AMD is an eye condition that occurs with aging. There are usually no obvious causes for this condition. However AMD affects the macula severely after the age of 50 leading to vision loss.
Age related macular degeneration or AMD is an eye condition that occurs with aging. There are usually no obvious causes for this condition. However AMD affects the macula severely after the age of 50 leading to vision loss.
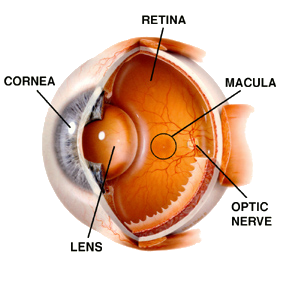
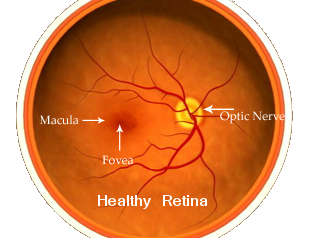
The retina and the macula
The retina is a curtain of cells that line the back of the eye. It is made up of special light sensitive cells called rods and cones. Light enters the eyes and passes through the lens which focuses the light on to the retina. The light causes electrochemical changes in the retinal cells leading to stimulation of the nerve cells supplying the retina. These nerve cells via the optic nerve carry the visual information to the brain that allows us to see an image. The retina contains the retinal pigment epithelium (RPE), the rods and cone cells and an inner lining Bruch’s membrane.
The macula is the small part or spot that lies near the centre of the retina. The macula is where the vision is focused and is the best point of vision. The central and most important part of the macula is called the fovea. The outer part of the retina is responsible for peripheral vision.
Causes
AMD is one of the commonest forms of irreversible visual loss in patients over 50 years of age worldwide. 10% of 65-75 year-olds and 30% of over 75 year-olds are found to be affected to a certain degree with this condition. 1.7% of the population over 50 years of age in addition has severe disease and 18% of population over 85 have severe AMD. With rise of aging population, AMD incidence is on the rise.
Risk factors that increase the chances for AMD include :
- Increasing age
- Smoking is one of the well know risk factors for AMD
- There is some evidence that presence of hypermetropia or far sightedness may be a risk factor for AMD.
- Those with a previous cataract surgery may also be at a risk of AMD.
- Patients who have high blood pressure may also be at a high risk of developing AMD. Diabetes however is not a risk factor for AMD.
- Genes may play a role in risk of AMD. Some genes that run in families may be responsible for increased risk of AMD.
Similar to genetic link, ethnicity, gender and race are also associated with risk of AMD. White and Chinese people are more commonly affected than others while blacks are least affected. Women are said to be more affected in over 75 year-olds.
Pathology of AMD
In AMD the macula of the retina is affected. There is deposition of small collections of chemicals also called colloid bodies and commonly known as drusen. The drusen is deposited in the region between the retinal pigment epithelium (RPE) and the underlying Bruch’s membrane.
The changes are uncommon before the age of 45 years and as the persons ages the number and size of these drusen rises.
In early stages these changes in the retina are called age-related maculopathy (ARM). After the changes reach a critical size in the macula, they are termed as age-related macular degeneration (AMD).
Symptoms
Age-related macular degeneration (AMD) may present with several initial symptoms that lead to progressive vision loss. Some of these symptoms include
- Difficulty in tasks that require visual focus like reading, driving and recognising faces
- There may be flashing lights. This is called photopsia or flickering or flashing lights
- Night glares
- Presence of floaters in the visual field
- Visual hallucinations may be present. This is also called Charles Bonnet syndrome
- Abnormal and reduced night vision
- In atrophic or dry AMD things may appear smaller or bigger than they are. This is called micropsia or macropsia respectively.
- In wet AMD there is profound central vision loss that may be sudden in case of bleeding
Diagnosis
While diagnosing AMD, certain eye disorders need to be ruled out. These include cataract, refractive errors, corneal disease, retinal detachment, stroke, brain tumors etc. For diagnosis the vision and refraction is tested followed by slit-lamp examination or bio-microscopy. This helps view the structures of the eye in detail. Another test Optical coherence tomography (OCT) is now commonly used to confirm the diagnosis. This shows the structures of the retina. Patients with suspected proliferative changes may also need fluorescein angiography to assess the extent of damage.
Treatment of AMD
The aim of treatment of AMD is to minimise visual loss in the early stages and to retain maximum possible vision. There is no effective treatment for dry AMD. In patients with wet AMD the formation of new blood vessels has been the target of medications that are being developed.
Complication
Despite treatment, most patients with AMD develop progressive loss of vision. About 80% of patients slowly become blind.
Some of the other complications include:
- detachment and tearing of the retina
- bleeding in the eye
- Severe eye infections
- Cataract etc.